Articles
- Page Path
- HOME > J Educ Eval Health Prof > Volume 18; 2021 > Article
-
Review
E-learning in health professions education during the COVID-19 pandemic: a systematic review -
Aziz Naciri1*
 , Mohamed Radid2,3
, Mohamed Radid2,3 , Ahmed Kharbach4,5
, Ahmed Kharbach4,5 , Ghizlane Chemsi1,3
, Ghizlane Chemsi1,3
-
DOI: https://doi.org/10.3352/jeehp.2021.18.27
Published online: October 29, 2021
1Multidisciplinary Laboratory in Sciences and Information, Communication and Education Technology, Faculty of Sciences Ben M’Sik, Hassan II University of Casablanca, Casablanca, Morocco
2Laboratory of Physical Chemistry of Materials, Faculty of Sciences Ben M’Sik, Hassan II University of Casablanca, Casablanca, Morocco
3Observatory of Research in Interdisciplinary Didactics and University Pedagogy, Faculty of Sciences Ben M’Sik, Hassan II University of Casablanca, Casablanca, Morocco
4Laboratory of Biostatistics, Clinical Research and Epidemiology, Faculty of Medicine and Pharmacy of Rabat, Mohamed V University, Rabat, Morocco
5High Institute of Nursing Professions and Technical Health, Agadir, Morocco
- *Corresponding email: aziz.naciri-etu@etu.univh2c.ma; aziz.ncr@gmail.com
© 2021 Korea Health Personnel Licensing Examination Institute
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- As an alternative to traditional teaching, e-learning has enabled continuity of learning for health professions students during the coronavirus disease 2019 (COVID-19) pandemic. This review explored health professions students; perceptions, acceptance, motivation, and engagement with e-learning during the COVID-19 pandemic. Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, a systematic review was conducted by consulting 5 databases: PubMed, ERIC (Ebsco), Science Direct, Scopus, and Web of Science. The quality of the included studies was assessed using the Medical Education Research Study Quality Instrument. The research protocol was previously registered in the PROSPERO registry (CRD42021237055). From 250 studies identified, 15 were selected with a total of 111,622 students. Mostly positive perceptions were reported in 7 of 12 studies, which mainly focused on technology access, possession of basic computer skills, pedagogical design of online courses, online interactions, and learning flexibility. However, predominantly negative perceptions were identified in 5 of 12 studies, which pointed out constraints related to internet connections, the use of educational platforms, and acquisition of clinical skills. Satisfactory levels of acceptance of distance learning were reported in 3 of 4 studies. For student motivation and engagement, 1 study reported similar or higher motivation than with traditional teaching, and another study indicated that student engagement significantly increased during the COVID-19 pandemic. Health professions students showed a positive response to e-learning regarding perceptions, acceptance, motivation, and engagement. Future research is needed to remediate the lack of studies addressing health professions students’ motivation and engagement during the COVID-19 pandemic.
- Rationale
- On March 11, 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) to be a pandemic disease [1]. This urgent and unexpected situation has caused unprecedented challenges to health systems, especially in the health sciences education sector, where concerns have been raised regarding the possibility that medical and nursing students could contract COVID-19 during their training and become potential transmitters of the virus in health care institutions. In the context of this crisis, changes in the teaching-learning paradigm have become an unavoidable necessity [2]. E-learning is an important alternative to ensure continuity of learning while protecting students against the risk of COVID-19 infection in the campus environment [3]. Indeed, e-learning is a teaching approach based on digital media and devices as tools to improve access to training, communication, and interactions between teachers and students [4]. It is a relatively new and growing approach in health professions education [5]. This pedagogical model offers a flexible learning environment where students can learn at their own pace without time or space constraints through various educational content (text, image, audio, and video). When using e-learning platforms, students interact with teachers, educational content, and technological innovations [6].
- However, the sudden transition to distance learning during COVID-19, combined with the concomitant time constraints, prevented the effective implementation of e-learning [5]. Furthermore, some teachers had limited skills in e-learning-based pedagogical methods [7]. A lack of motivation and absence of interactions between teachers and students were also pointed out as the main disadvantages [8].
- Objectives
- The purpose of this review was to explore health science students’ perceptions, acceptance, motivation, and engagement with e-learning during the COVID-19 pandemic. The specific research questions were as follows: (1) What are students’ perceptions of the implementation of e-learning during the COVID-19 pandemic? (2) Did heath profession students accept the adoption of e-learning during COVID-19? (3) What is the motivational level of health professions students towards e-learning during the COVID-19 crisis? (4) What is the engagement level of students during the transition to e-learning during COVID-19?
Introduction
- Ethics statement
- This was not a human-subject study; therefore, neither approval by the institutional review board nor obtainment of the informed consent was required.
- Registration and protocol
- This systematic literature review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [9]. The research protocol was previously registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42021237055; available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021237055).
- Eligibility criteria
- Inclusion and exclusion criteria were developed using the population, intervention, comparison, outcome, and study design (PICOS) framework (Table 1).
- Information sources
- PubMed, ERIC (Ebsco), Science Direct, Scopus, and Web of Science databases were checked for English-language studies published from March 11, 2020, to February 10, 2021. The databases were last accessed on February 11, 2021.
- Search strategy
- The database searches (PubMed, ERIC [Ebsco], Science Direct, Scopus, and Web of Science) were conducted independently by 2 authors (A.N., A.K.), using the following keywords: (e-Learning) or (online learning) or (distance learning) or (distance education) and (medical education) or (nurs* education) and (COVID-19) or (2019-novel coronavirus) or (2019-nCoV) or (SARS-CoV-2). Examples of the search terms are as follows:
Scopus:
(TITLE-ABS (e-learning OR "online learning" OR "distance learning" OR "distance education")) AND (TITLE-ABS ("medical education" OR "nurs* education")) AND (TITLE-ABS (covid-19 OR "2019-novel coronavirus" OR 2019-ncov OR sars-cov-2))
PubMed:
((e-Learning[Title/Abstract] OR "online learning"[Title/Abstract] OR "distance learning"[Title/Abstract] OR "distance education"[Title/Abstract]) AND ("medical education" [Title/Abstract] OR "nursing education"[Title/Abstract])) AND (covid-19 [Title/Abstract] OR "2019-novel coronavirus" [Title/Abstract] OR 2019-ncov [Title/Abstract] OR sars-cov-2[Title/Abstract]).
- Selection process
- Two authors (A.N. and A.K.) eliminated duplicate articles using EndNote X9 (Clarivate, Philadelphia, PA, USA). They independently checked titles and abstracts to identify potentially included studies. This selection and filtering process was performed using Rayyan QCRI (Rayyan Systems Inc., Cambridge, MA, USA), a web and mobile application for systematic reviews [10]. In cases of persistent disagreement between the 2 authors, a third reviewer (G.C.) was requested to make a final decision. The full texts of the included articles were downloaded for further evaluation, and the reference lists of all relevant articles were reviewed to identify additional literature.
- Data collection process
- One author (A.N.) collected the data from the selected studies using an extraction form prepared in consensus between the authors. Another author (A.K.) verified the collected information. In case of any disagreement, a third author was consulted for a final decision.
- Data items
- Data were extracted on the following general characteristics of the selected studies: authors, year, country of provenance, study design, participants’ characteristics (discipline, age, gender), and educational platforms used. Moreover, data on students’ perception, acceptance, motivation, and engagement (mean or median scores or effective/percentage) towards e-learning were extracted. The measurement instruments used (items and domains) were also selected.
- Study risk of bias assessment
- The risk of bias assessment of the included studies was conducted independently by 2 authors (A.N. and M.R.) using the Medical Education Research Study Quality Instrument (MERSQI). The MERSQI is a tool for assessing the methodological quality of quantitative research articles. The scale consists of 10 items organized into 6 domains: study design, sampling, data types, validity of the assessment instrument, data analysis, and outcomes. The total score ranges from 5 to 18. The agreement between the 2 examiners’ results was analyzed using the kappa statistical coefficient (κ).
- Synthesis methods
- The data were classified and analyzed to achieve the objectives of the review. Students’ perceptions were extracted and tabulated with key items such as technology access, possession of basic computer skills, instructional design of online courses, online interactions, learning flexibility, health issues, and acquisition of clinical knowledge during online learning. Data synthesis was initially conducted by the first author (A.N.) and then was discussed with 2 other authors (A.K. and G.C.). The included studies were analyzed through a narrative synthesis. Due to the disparity and heterogeneity among studies’ results, a meta-analysis was not performed.
- Reporting bias assessment
- Reporting bias in this systematic review was assessed independently by 2 authors (A.N. and A.K.) in terms of selective outcome reporting by comparing study results with previously published study protocols and registrations. Any disagreement was resolved by consulting the opinion of a third author (G.C.).
- Certainty assessment
- Not done.
Methods
- Study selection
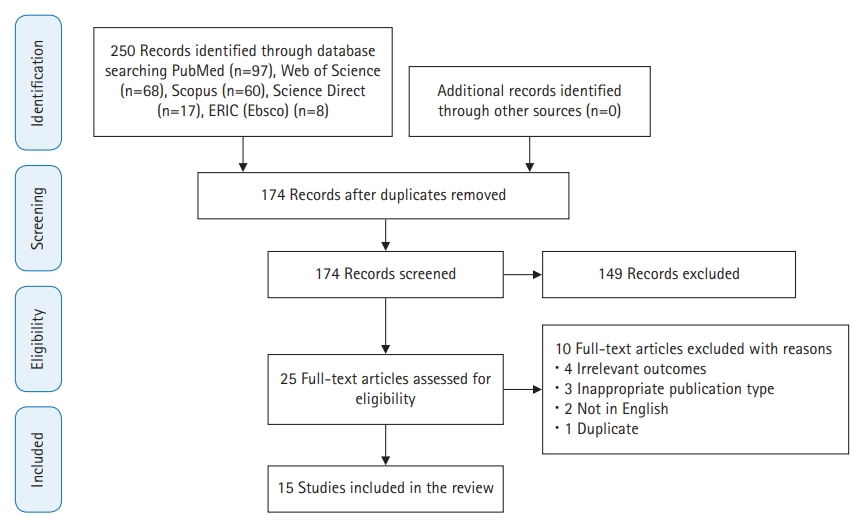
- The search strategy identified a total of 250 articles, of which 76 were duplicates. Of the 174 studies that were screened by title and abstract, 149 were excluded. The 25 studies that were eventually eligible were downloaded for a full review. Finally, 15 studies were included in this review [11-25]. The PRISMA flow chart illustrates the selection process of the included studies (Fig. 1).
- Study characteristics
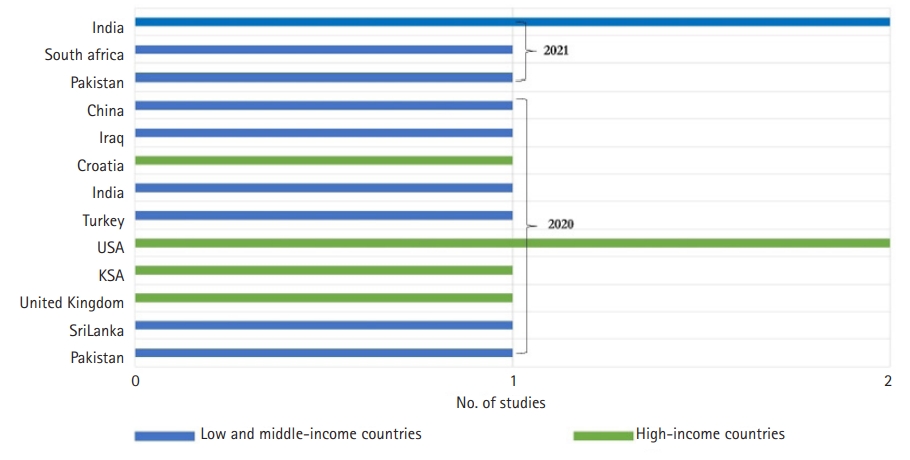
- Fifteen studies were considered eligible for this review. One-third of the studies were conducted in high-income countries [15,17,18,21,23], and two-thirds in low- and middle-income countries [11-14,16,19,20,22,24,25] (Fig. 2). The total number of participants was 111,622. The sample size of the studies ranged from 30 [18,23] to 99,559 students [25]. A total of 106,152 participants (95.1%) were medical students, as reported in 10 studies [14-20,23-25]. One study included 60 nursing students [13]. In other studies, the focus was on heterogeneous samples in terms of discipline. Two studies involved 4,745 medical and nursing students [21,22], while 2 other investigations sampled 665 medical and dental students [11,12]. The gender of participants was reported in 8 studies [11-13,15,17,22,23,25]. The gender ratio of the included studies ranged from 0.3 [23] to 0.71 [13]. Almost half of the studies were conducted among undergraduate students [12-16,19,22].
- All studies adopted fully online courses. The teaching platforms used were explicitly indicated in 8 studies [13,14,17-20,23,24]. Moodle was used in 2 studies [13,19], Zoom in 2 other studies [18,20], and WebEx video conferencing in 1 study investigation [23]. One study used both Zoom and Facebook as a freely accessible social media platform [14], and another opted for Zoom and Blackboard [17]. Google Classroom and Free Conference Call software were used in another study [24].
- Students’ perceptions were investigated by 9 studies [11-13,16,18,20,23-25] and acceptance by 3 studies [14,19,22]. In addition, 1 investigation tested students’ perceptions and motivation [21], 1 study tested perceptions and acceptance [17], and 1 article discussed students’ perceptions and engagement [15] (Table 2).
- Risk of bias in studies
- The methodological quality of half of the included studies as assessed by the MERSQI scale was relatively moderate, with a mean score of 8.50±1.44 and a median score of 8.50 (interquartile range, 7.5–9.5). The MERSQI score of the studies ranged from 6 [14] to 11.5 points [25], out of a total of 18. The kappa coefficient of concordance was 0.77. All included studies were cross-sectional studies with no control group, and participants were limited to fully online learning. The majority of studies used questionnaires developed by the authors. Furthermore, the response rate was less than 50% in 9 studies [11-17,20,24], and ranged from 50% to 74% in 6 studies [18,19,21-23,25]. The data analysis in 6 studies was limited to a descriptive level [14,16,18,21,23,24] (Table 3).
- Results of individual studies
- Relevant data from the included studies are grouped and summarized separately in Table 2 and Supplement 1.
- Results of syntheses
- Twelve of the 15 included studies examined students’ perceptions of e-learning during the COVID-19 pandemic, either in isolation or in addition to another parameter [11-13,15-18,20,21,23-25]. The measurement tools were developed principally by the authors, which led to different results due to heterogeneity in the items. The items were mainly related to major aspects of e-learning (technology access, possession of basic computer skills, pedagogical design of online courses, online interactions, learning flexibility, health issues, and acquisition of clinical knowledge during online learning). Positive perceptions of e-learning were predominantly recorded in 7 studies, including a total of 3,863 students [12,13,17,18,20,21,23]. Four studies (57.2%) were conducted among medical students [17,18,20,23], 1 among medical and dental students [12], 1 among medical and nursing students [21], and 1 exclusively among nursing students [13]. Four studies were conducted in high-income countries [17,18,21,23].
- A study by Kumar et al. [20] in 2020 compared students’ perceptions of a synchronous and an asynchronous course. Students’ perception scores were better for the direct classroom course than the online sessions (47.5±2.61 versus 35.5±3.25, P<0.001) [20]. Otherwise, the positive perceptions described by most students in other studies were related to technology access, possession of computer skills, online course design, online interactions and learning flexibility. Positive perceptions were reported for access to technological equipment in 3 studies (76.7% to 86%) [12,21,23], the possession of basic computer skills in 3 studies (51.2% to 84.7%) [12,17,21] and the instructional design of online courses in 6 studies, including an attractive learning content in 4 studies (48.8% to 84.2%) [12,13,17,21] and video learning in 3 investigations (58.1% to 89.7%) [12,18,21]. Moreover, 3 studies revealed positive perceptions of interactions on the platform (69.5% to 86.7%) [17,21,23] and learning flexibility in 4 studies (52.3% to 100%) [12,17,18,23]. Otherwise, mainly positive perceptions of e-learning were mentioned in 5 studies [11,15,16,24,25]. Four of these studies were conducted among medical students [15,16,24,25], and 1 study was conducted among medical and dental students [11]. Most of these studies (80%) were performed in low- and middle-income countries [11,16,24,25].
- Negative perceptions in the included studies focused on access to the internet in 2 studies (21.5% to 35.9%) [15,16], health problems caused by the use of e-learning in 2 studies (62.5% to 67%) [18,24], and difficulty in developing clinical skills online in 2 studies (82.2% to 84.2%) [15,17]. The results are presented in more detail in Supplement 1.
- Among the 15 included studies, students’ acceptance of e-learning was investigated in 4 studies, with a total sample size of 4,553 participants [14,17,19,22]. Three (75%) of these 4 studies were conducted among medical students exclusively [14,17,19], and 1 was conducted among medical and nursing students [22]. Three-quarters of these studies were conducted in low- and middle-income countries [14,19,22].
- Singh et al. [22] in 2021 approached e-learning acceptance by exploring 4 components. The first was related to the feasibility/practicality of online courses, including internet connectivity, device logistics, internet and computer literacy, and the availability of a dedicated space for participating in online classes. The second was associated with health issues during online courses. The third was about online teaching methods, including the type of teaching methods and class time allocation. The fourth dealt with students’ attitudes towards e-learning and their preferences. In this context, Singh et al. [22] in 2021 reported that 18.2% of students had a personal desktop/laptop computer, and those from affluent families and those living in cities had better access to e-learning facilities (internet connectivity, availability of a personal computer, a dedicated room, and training in computer/internet use). PowerPoint presentations were the most frequently used teaching method (80%). Loss of concentration (58.1%), eye strain (54%), and sleep disturbance (42.8%) were the most common health problems among students who attended classes for more than 4 hours per day. Moreover, there was insufficient interaction time with the instructor (30%). Regarding students’ attitudes and preferences towards e-learning, less than a quarter (20.4%) of the participants felt that online learning could replace traditional teaching (15% of medical students versus 30% of nursing students, P=0.001). Students expressed preferences for 3–6 classes per day, with each lasting for <40 minutes and a 10- to 20-minute break between classes and/or interactive sessions [22].
- Two other studies reported moderate levels of e-learning acceptance [17,19]. The study conducted by Ibrahim et al. [17] in 2020 reported a mean score of 102.82±24.10 (min: 21, max: 147) using the E-Learning Acceptance Measure, which was composed of 3 components: tutor quality (with a mean score of 39.34±10.14), perceived usefulness (with a mean score of 44.11±11.52), and facilitating conditions (with a mean score of 19.36±5.85). Moreover, a second investigation conducted by Kolcu et al. [19] in 2020 highlighted a total score of 56.99% using the Learning Management System Acceptance Scale, which contained 4 sub-dimensions: performance expectancy (56.75%), effort expectancy (62.00%), facilitating conditions (59.68%), and social influence (44.67%).
- Similarly, Chandrasinghe et al. [14] in 2020 reported very satisfactory levels of acceptance regarding the relevance of the topics studied (90%), the importance of the topics (89%), interactions within the platform (87.1%), the improvement of interest in clinical medicine (79.3%), the acquisition of skills and understanding of topics (88%), and the importance of the topics covered in examinations and clinical practice (90%).
- Motivation in a distance learning environment during the COVID-19 pandemic was tested in 1 study [21]. This study was conducted at 9 health science institutions with 2,520 medical and nursing students. Student motivation was measured by a questionnaire developed by the authors with 2 items. The first item focused on motivation to participate in online learning compared to classroom courses, and 64.4% of participants demonstrated an equal or higher motivational level to attend exclusive e-learning. The second item related to student motivation during the progression of online courses, and more than half of participants (65.5%) reported an equal or higher level of motivation to participate in a longer duration of exclusive e-learning.
- Student engagement was reported in 1 study that was conducted among 2,721 medical students [15]. Student engagement was measured by a questionnaire developed by the authors through an analysis of the number of hours spent on e-learning during the COVID-19 pandemic compared to traditional teaching before the pandemic. Students spent an average of 7–10 hours using e-learning platforms during the pandemic, compared to 4–6 hours before the pandemic (P<0.05). Similarly, the number of students spending more extended periods on online teaching platforms significantly increased during the COVID-19 health crisis. Furthermore, small group work methods, group discussions, online case simulations, and quizzes helped increase student engagement [15].
- Reporting biases
- The search showed that no protocols or records of the included studies were previously published. The risk of reporting bias was unclear because it was not possible to determine whether all the results were included in the published reports.
Results
Students’ perceptions
Students’ acceptance
Students’ motivation
Students’ engagement
- Summary of evidence
- This systematic review explored the different aspects of health science students’ perceptions, acceptance, motivation, and engagement with e-learning during the COVID-19 pandemic. The majority of studies reported positive perceptions of e-learning. These results are similar to the findings of literature reviews conducted before and during the COVID-19 pandemic [26-28]. However, Xhelili et al. [29] in 2021 found positive perceptions of traditional learning during the COVID-19 pandemic by Albanian university students. The participants in that study reported difficulties related principally to the unavailability of internet connection and the lack of technological devices.
- In our review, the positive trend in perceptions of distance learning may be due primarily to the sudden and unexpected shift to e-learning, which generated a sense of security among students during the spread of the virus. This situation probably caused a forced adaptation to the online learning requirements to ensure continuity of learning during these exceptional times. Second, positive perceptions could also be explained by remarkable advances in recent years in computer-based platforms in health sciences education, which have progressed to the point that they offer a learning climate similar to face-to-face teaching. Furthermore, technology access, computer skills, pedagogical engineering quality of online courses, and learning flexibility were the main items associated with positive perceptions of e-learning. Nevertheless, limited internet connection, technical problems in using educational platforms, and difficulties in acquiring clinical skills were the most important constraints and limitations reported by students in online learning. Consistent findings have been reported in other studies conducted during the pandemic [29-32].
- Satisfactory levels of e-learning acceptance were expressed by health professions students during the COVID-19 pandemic. Other studies supported this finding [33,34]. Nevertheless, a previous study conducted by Ngampornchai and Adams [35] in 2016, using the unified theory of acceptance and use of technology, reported that students had a cautious tendency to accept online learning. Performance expectancy and effort expectancy were strong indicators of technology acceptance. The predisposition to accept distance learning courses in the current study could be attributed, on the one hand, to the usability of e-learning platforms. On the other hand, the concordance between the educational content of health sciences training and didactic conceptions of courses (video learning, serious games) may be a contributor. Taat and Francis [33] in 2020 showed that usability and ease of use platforms, lecturer characteristics, system quality, the information provided, and available technical support were the main factors influencing the acceptance of e-learning.
- With regard to students’ motivation, our review found an equal or higher motivation to attend exclusive e-learning compared to classroom learning. This result is in agreement with previous studies’ findings [36-38]. However, Aguilera-Hermida et al. [39] in 2021 demonstrated a decrease in students’ motivational levels in Mexico, Peru, and the United States after switching to e-learning during the COVID-19 pandemic and a significantly unchanged motivational level in Turkish students. This study also reported that lower motivation in students in the United States, Peru, and Mexico during online learning was associated with worse cognitive engagement. In the current review, the significant observed improvement in motivation in a digital environment could be related to the temporospatial flexibility of the pedagogical content, accessibility, and technological skills [40].
- Regarding student engagement, the only study included that investigated this parameter showed a statistically significant difference between the number of hours spent on e-learning before and during the pandemic. This result is corroborated by the exclusive and massive adoption of e-learning during the confinement and post-confinement periods of several waves of outbreaks of COVID-19 variants. This finding of our review contradicts those of other studies conducted during the COVID-19 pandemic [41,42]. Wester et al. [41] in 2021 reported a significant decrease in the overall engagement score calculated from students’ behavioral, cognitive, and emotional engagement scores during the pandemic. Moreover, Chan et al. [42] in 2021 found that 55% of nursing students were not highly engaged in an online course during the COVID-19 pandemic. Psychological motivation, peer collaboration, cognitive problem solving, interaction with instructors, community support, and learning management are factors that can improve student engagement in a digital environment [43].
- Limitations
- This review has some limitations. First, all included studies were cross-sectional. Second, the authors used various measurement instruments, and the consequent disparity among items made an integrative analysis difficult. Third, student motivation and engagement were measured in the included studies through 2 items for each. In addition, a certainty assessment was not performed. Therefore, we must be cautious in interpreting the results. The last limitation is that non-English-language articles were not reviewed.
- Implications for practice and future research
- The results of this review encourage decision-makers in the health professions education field to integrate e-learning into training programs by ensuring, on the one hand, equitable access to technological equipment and internet connections and, on the other hand, developing students’ computer skills. Furthermore, pedagogical approaches based on digital teaching could be beneficial as an alternative or complement to traditional teaching. If this method had been adopted before in health professions education, institutions could have more easily overcome the unprecedented challenges caused by the emergence of this COVID-19 crisis. Therefore, investment in the implementation of e-learning remains an unavoidable necessity because the return on investment could be decisive in terms of the quality of training received by health science students and consequently to the health services provided to the population. Moreover, the data explored in this study showed a lack of evidence, especially for students’ motivation and engagement with e-learning during the COVID-19 pandemic. Further methodologically rigorous research is needed, especially in the Middle East/North Africa region, to help fill this gap. It is also essential to investigate the problems of failure and dropout in health professions education in relation to online learning during this pandemic.
Discussion
- Switching to online learning to ensure the continuity of learning during the COVID-19 pandemic was challenging for health professions education programs. The findings of this study indicate that the emergency shift to online health science learning during this health crisis received positive feedback from students in terms of perceptions, acceptance, motivation, and engagement. Although the socio-economic contexts of the countries differed, online learning was consistently facilitated by some major elements such as technology access, possession of basic computer skills, pedagogical design of online courses, and learning flexibility. In contrast, students reported constraints including access to internet connections, the use of educational platforms, and the acquisition of online clinical skills. These results should be noted in order to integrate these devices better into educational programs.
Conclusion
-
Authors’ contributions
Conceptualization: AN, MR, GC. Data curation: AN, AK. Methodology, Formal analysis, validation: AN, AK, MR. Funding acquisition: not applicable. Writing–original draft: AN, GC. Writing–review & editing: AN, MR, AK, GC.
-
Conflict of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Data availability
None.
Article information
Acknowledgments
Supplementary materials
| Study (year) | Country | Study design | Discipline | No. of participants | Instructional design | Used platform | Results | Measurement instruments | Main domains and/or items of questionnaire |
|---|---|---|---|---|---|---|---|---|---|
| Abbasi et al. [11] (2020) | Pakistan | CSS | Medicine and dentistry | Medical students: 204 | Fully online course | NR | P | 23-item questionnaire, developed by the authors (5-point Likert scale) | Future learning preferences, comparison of e-learning with traditional teaching, quality and impact of e-learning, student-teacher interactions, online teaching security |
| Dental students: 178 | |||||||||
| Anwar et al. [12] (2021) | Pakistan | CSS | Medicine and dentistry | 283 | Fully online course | NR | P | 20-item questionnaire, developed by the authors based on the original version of Watkins and his colleagues (5-point Likert scale) | Technology access, online skills and relationships, students’ views and students’ perceptions of possible advantages of e-learning |
| Buthelezi et al. [13] (2021) | South Africa | CSS | Nursing | 60 | Fully online course | Moodle | P | Questionnaire with 23 items, designed by the authors (4-point Likert scale) | Computer access, frequency of use, prior exposure to e-learning platforms, anxiety and attitude towards technology, perceived computer self-efficacy |
| Chandrasinghe et al. [14] (2020) | Sri Lanka | CSS | Medicine | 1,047 | Fully online course | Zoom, Facebook | A | Questionnaire designed by the authors | Relevance and importance of the topic, students’ discussions and clinical sense, discussion and knowledge and understanding of the topic |
| Dost et al. [15] (2020) | UK | CSS | Medicine | 2,721 | Fully online course | NR | P/E | 20-item questionnaire, developed by the authors based in part on the Ready Education Environment Measure (5-point Likert scale) | The use and experience of online teaching during the COVID-19 pandemic, perceived benefits and barriers of online teaching |
| Gupta et al. [16] (2021) | India | CSS | Medicine | 248 | Fully online course | NR | P | 22-item online survey developed by the authors (5-point Likert scale) | Time spent on online and offline learning, modality of didactic learning, interaction with educators, facilitating and hindering factors during online classes, comparison of e-learning with traditional teaching, the features preferred during online classes |
| Ibrahim et al. [17] (2020) | Saudi Arabia | CSS | Medicine | 340 | Fully online course | Zoom, Blackboard | P/A | 21-item data collection sheets from the E-Learning Acceptance Measure and items to assess student perception (7-point Likert scale) | Preferred learning management system, tutor quality, perceived usefulness, facilitating conditions, perceptions regarding the benefits, enablers, and barriers to e-learning |
| Kivlehan et al. [18] (2020) | USA | CSS | Medicine | 30 | Fully online course | Zoom | P | Questionnaire developed by the authors | Perceived benefits and barriers to e-learning, satisfaction with education during the COVID-19 pandemic |
| Kolcu et al. [19] (2020) | Turkey | CSS | Medicine | 941 | Fully online course | Moodle | A | 21-item questionnaire from the Learning Management System Acceptance Scale (5-point Likert scale) | Performance expectancy, effort expectancy, facilitating conditions, social influence |
| Kumar et al. [20] (2020) | India | CSS | Medicine | 600 | Fully online course | Zoom | P | 10-item questionnaire developed by the authors (5-point Likert scale) | Flexibility of learning, achievement of pedagogical objectives, attractivity of the online course |
| Puljak et al. [21] (2020) | Croatia | CSS | Medicine and nursing | 2,520 | Fully online course | NR | P/M | 73-item questionnaire developed by the authors (5-point Likert scale) | Personal experience with e-learning, motivation and attendance, possibility to participate in e-learning, continuation of education during the pandemic |
| Singh et al. [22] (2021) | India | CSS | Medicine and nursing | Medical student: 1,541 | Fully online course | NR | A | 33-item survey, developed by the authors (dichotomous and multiple-choice questions) | Feasibility of online classes, health issues arising from online classes, methods of online teaching, student preferences and attitudes towards e-learning |
| Nursing student: 684 | |||||||||
| Singhi et al. [23] (2020) | USA | CSS | Medicine | 30 | Fully online course | WebEx | P | 19-item survey designed by the authors | Ease of technical access to the online platform, level of comfort with participation, knowledge acquisition, wellness, and COVID-19-specific coverage |
| Tuma et al. [24] (2020) | Iraq | CSS | Medicine | 636 | Fully online course | Google Classroom, Free Conference Call | P | 10-item survey, designed by the authors | The feasibility of educational technology platforms for distance education and the education’s perceived quality |
| Wang et al. [25] (2020) | China | CSS | Medicine | 99,559 | Fully online course | NR | P | 20-item questionnaire developed by the authors based in part on the technology acceptance model (5-point Likert scale) | Prior online learning experiences, perceptions of ongoing online education |
| Study | Study design |
Sampling |
Type of data |
Validity of the evaluation instrument |
Data analysis |
Outcome |
Total score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Institution studied | Response rate score | Internal structure | content | Relationships to other variables | Appropriateness of analysis | Complexity of analysis | Satisfaction, attitudes, perceptions | Knowledge, skills | Behaviors | Patient/health care outcome | ||||
| Abbasi et al. [11] | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 0 | 9 |
| Anwar et al. [12] | 1 | 0.5 | 0.5 | 1 | 0 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 0 | 8 |
| Buthelezi et al. [13] | 1 | 0.5 | 0.5 | 1 | 0 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 0 | 9 |
| Chandrasinghe et al. [14] | 1 | 0.5 | 0.5 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 6 |
| Dost et al. [15] | 1 | 1.5 | 0.5 | 1 | 0 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 0 | 8 |
| Gupta et al. [16] | 1 | 0.5 | 0.5 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 7 |
| Ibrahim et al. [17] | 1 | 0.5 | 0.5 | 1 | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 0 | 9 |
| Kivlehan et al. [18] | 1 | 0.5 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 7.5 |
| Kolcu et al. [19] | 1 | 0.5 | 1 | 1 | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 0 | 9.5 |
| Kumar et al. [20] | 1 | 0.5 | 0.5 | 1 | 0 | 1 | 0 | 1 | 2 | 1 | 1.5 | 0 | 0 | 9.5 |
| Puljak et al. [21] | 1 | 1.5 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 8.5 |
| Singh et al. [22] | 1 | 1.5 | 1 | 1 | 0 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 0 | 10.5 |
| Singhi et al. [23] | 1 | 0.5 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 7.5 |
| Tuma et al. [24] | 1 | 0.5 | 0.5 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 7 |
| Wang et al. [25] | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 0 | 11.5 |
- 1. World Health Organization. Director-General’s opening remarks at the media briefing on COVID-19 [Internet]. Geneva: World Health Organization; 2020 [cited 2021 Mar 10]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 2. United Nations. Policy Brief: education during COVID-19 and beyond [Internet]. New York (NY): United Nations; 2020 [cited 2021 Apr 12]. Available from: https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2020/08/sg_policy_brief_covid-19_and_education_august_2020.pdf
- 3. Fan C, Li M, Li X, Zhu M, Fu P. Who got infected with COVID-19?: a study of college students in Wuhan (China). Int J Environ Res Public Health 2021;18:2420. https://doi.org/10.3390/ijerph18052420 ArticlePubMedPMC
- 4. Sangra A, Vlachopoulos D, Cabrera N. Building an inclusive definition of e-learning: an approach to the conceptual framework. Int Rev Res Open Distrib Learn 2012;13:145-159. https://doi.org/10.19173/irrodl.v13i2.1161 Article
- 5. O’Doherty D, Dromey M, Lougheed J, Hannigan A, Last J, McGrath D. Barriers and solutions to online learning in medical education: an integrative review. BMC Med Educ 2018;18:130. https://doi.org/10.1186/s12909-018-1240-0 ArticlePubMedPMC
- 6. Castro MD, Tumibay GM. A literature review: efficacy of online learning courses for higher education institution using meta-analysis. Educ Info Technol 2021;26:1367-1385. https://doi.org/10.1007/s10639-019-10027-z Article
- 7. Stanistreet P, Elfert M, Atchoarena D. Education in the age of COVID-19: understanding the consequences. Int Rev Educ 2021;1-7. https://doi.org/10.1007/s11159-020-09880-9 ArticlePubMedPMC
- 8. Panchabakesan S. Problems and prospectives in distance education in India in the 21st century. Probl Educ 21st Century 2011;30:113-122. Article
- 9. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hrobjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71 ArticlePubMedPMC
- 10. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan: a web and mobile app for systematic reviews. Syst Rev 2016;5:210. https://doi.org/10.1186/s13643-016-0384-4 ArticlePubMedPMC
- 11. Abbasi S, Ayoob T, Malik A, Memon SI. Perceptions of students regarding E-learning during COVID-19 at a private medical college. Pak J Med Sci 2020;36:S57-S61. https://doi.org/10.12669/pjms.36.COVID19-S4.2766 ArticlePubMedPMC
- 12. Anwar A, Mansoor H, Faisal D, Khan HS. E-Learning amid the COVID-19 lockdown: standpoint of medical and dental undergraduates. Pak J Med Sci 2021;37:217-222. https://doi.org/10.12669/pjms.37.1.3124 ArticlePubMedPMC
- 13. Buthelezi LI, Van Wyk JM. The use of an online learning management system by postgraduate nursing students at a selected higher educational institution in KwaZulu-Natal, South Africa. Afr J Health Prof Educ 2020;12:211-214. https://doi.org/10.7196/ajhpe.2020.v12i4.1391 Article
- 14. Chandrasinghe PC, Siriwardana RC, Kumarage SK, Munasinghe BN, Weerasuriya A, Tillakaratne S, Pinto D, Gunathilake B, Fernando FR. A novel structure for online surgical undergraduate teaching during the COVID-19 pandemic. BMC Med Educ 2020;20:324. https://doi.org/10.1186/s12909-020-02236-9 ArticlePubMedPMC
- 15. Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open 2020;10:e042378. https://doi.org/10.1136/bmjopen-2020-042378 ArticlePubMed
- 16. Gupta S, Dabas A, Swarnim S, Mishra D. Medical education during COVID-19 associated lockdown: faculty and students’ perspective. Med J Armed Forces India 2021;77(Suppl 1):S79-S84. https://doi.org/10.1016/j.mjafi.2020.12.008 Article
- 17. Ibrahim NK, Al Raddadi R, AlDarmasi M, Al Ghamdi A, Gaddoury M, AlBar HM, Ramadan IK. Medical students’ acceptance and perceptions of e-learning during the COVID-19 closure time in King Abdulaziz University, Jeddah. J Infect Public Health 2021;14:17-23. https://doi.org/10.1016/j.jiph.2020.11.007 ArticlePubMed
- 18. Kivlehan E, Chaviano K, Fetsko L, Javaid S, Chandan P, Rojas AM, Dubon ME. COVID-19 pandemic: early effects on pediatric rehabilitation medicine training. J Pediatr Rehabil Med 2020;13:289-299. https://doi.org/10.3233/PRM-200765 ArticlePubMed
- 19. Kolcu G, Baser Kolcu MI, Demir S, Gulle K. Evaluation of learning management system in medical education in time of COVID-19. Prog Nutr 2020;22(2-S):e2020005. https://doi.org/10.23751/pn.v22i2-S.10443 Article
- 20. Kumar S, Misra R, Chakraborty D, Chhabra PK, Upadhyaya P. A study of perceptions of students and teachers towards e-learning and its effectiveness: a cross-sectional study during COVID-19 lockdown in JNUIMSRC. Int J Cur Res Rev 2020;12:195-198. https://doi.org/10.31782/IJCRR.2020.122336 Article
- 21. Puljak L, Civljak M, Haramina A, Malisa S, Cavic D, Klinec D, Aranza D, Mesaric J, Skitarelic N, Zoranic S, Majstorovic D, Neuberg M, Miksic S, Ivanisevic K. Attitudes and concerns of undergraduate university health sciences students in Croatia regarding complete switch to e-learning during COVID-19 pandemic: a survey. BMC Med Educ 2020;20:416. https://doi.org/10.1186/s12909-020-02343-7 ArticlePubMedPMC
- 22. Singh HK, Joshi A, Malepati RN, Najeeb S, Balakrishna P, Pannerselvam NK, Singh YK, Ganne P. A survey of E-learning methods in nursing and medical education during COVID-19 pandemic in India. Nurse Educ Today 2021;99:104796. https://doi.org/10.1016/j.nedt.2021.104796 ArticlePubMedPMC
- 23. Singhi EK, Dupuis MM, Ross JA, Rieber AG, Bhadkamkar NA. Medical hematology/oncology fellows’ perceptions of online medical education during the COVID-19 pandemic. J Cancer Educ 2020;35:1034-1040. https://doi.org/10.1007/s13187-020-01863-6 ArticlePubMedPMC
- 24. Tuma F, Nassar AK, Kamel MK, Knowlton LM, Jawad NK. Students and faculty perception of distance medical education outcomes in resource-constrained system during COVID-19 pandemic: a cross-sectional study. Ann Med Surg (Lond) 2021;62:377-382. https://doi.org/10.1016/j.amsu.2021.01.073 ArticlePubMedPMC
- 25. Wang C, Xie A, Wang W, Wu H. Association between medical students’ prior experiences and perceptions of formal online education developed in response to COVID-19: a cross-sectional study in China. BMJ Open 2020;10:e041886. https://doi.org/10.1136/bmjopen-2020-041886 ArticlePubMedPMC
- 26. Maznik AK, Ribeiro DC, Baxter GD. Online technology use in physiotherapy teaching and learning: a systematic review of effectiveness and users’ perceptions. BMC Med Educ 2015;15:160. https://doi.org/10.1186/s12909-015-0429-8 ArticlePubMedPMC
- 27. Plch L. Perception of technology-enhanced learning by medical students: an integrative review. Med Sci Educ 2020;30:1707-1720. https://doi.org/10.1007/s40670-020-01040-w ArticlePubMedPMC
- 28. Layali K, Al-Shlowiy A. Students’ perceptions of e-learning for ESL/EFL in Saudi Universities at time of coronavirus: a literature review. Indones EFL J 2020;6:97-108. https://doi.org/10.25134/ieflj.v6i2.3378 Article
- 29. Xhelili P, Ibrahimi E, Rruci E, Sheme K. Adaptation and perception of online learning during COVID-19 pandemic by Albanian university students. Int J Stud Educ 2021;3:103-111. https://doi.org/10.46328/ijonse.49 Article
- 30. Ramachandran K, Kumar RD. Perception of medical students about online learning in the COVID-19 era. Biomedicine 2021;41:139-145. https://doi.org/10.51248/.v41i1.549 Article
- 31. Hebebci MT, Bertiz Y, Alan S. Investigation of views of students and teachers on distance education practices during the coronavirus (COVID-19) pandemic. Int J Technol Educ Sci 2020;4:267-282. https://doi.org/10.46328/ijtes.v4i4.113 Article
- 32. Baczek M, Zaganczyk-Baczek M, Szpringer M, Jaroszynski A, Wozakowska-Kaplon B. Students’ perception of online learning during the COVID-19 pandemic: a survey study of Polish medical students. Medicine (Baltimore) 2021;100:e24821. https://doi.org/10.1097/MD.0000000000024821 ArticlePubMedPMC
- 33. Taat MS, Francis A. Factors influencing the students’ acceptance of e-learning at teacher education institute: an exploratory study in Malaysia. Int J High Educ 2020;9:133-141. https://doi.org/10.5430/ijhe.v9n1p133 Article
- 34. Costa A, Costa A, Olsson I. Students’ acceptance of e-learning approaches in laboratory animal science training. Lab Anim 2019 Oct 20 [Epub]. https://doi.org/10.1177/0023677219879170 Article
- 35. Ngampornchai A, Adams J. Students’ acceptance and readiness for E-learning in Northeastern Thailand. Int J Educ Technol High Educ 2016;13:34. https://doi.org/10.1186/s41239-016-0034-x Article
- 36. Harandi SR. Effects of e-learning on students’ motivation. Procedia Soc Behav Sci 2015;181:423-430. https://doi.org/10.1016/j.sbspro.2015.04.905 Article
- 37. Na KS, Petsangsri S, Tasir Z. The relationship between academic performance and motivation level in e-learning among Thailand university students. Int J Inf Educ Technol 2020;10:184. https://doi.org/10.18178/ijiet.2020.10.3.1360 Article
- 38. Kew SN, Petsangsri S, Ratanaolarn T, Tasir Z. Examining the motivation level of students in e-learning in higher education institution in Thailand: a case study. Educ Inf Technol 2018;23:2947-2967. https://doi.org/10.1007/s10639-018-9753-z Article
- 39. Aguilera-Hermida AP, Quiroga-Garza A, Gomez-Mendoza S, Del Rio Villanueva CA, Avolio Alecchi B, Avci D. Comparison of students’ use and acceptance of emergency online learning due to COVID-19 in the USA, Mexico, Peru, and Turkey. Educ Inf Technol (Dordr) 2021 Apr 14 [Epub]. https://doi.org/10.1007/s10639-021-10473-8 Article
- 40. Kim KJ, Frick TW. Changes in student motivation during online learning. J Educ Comput Res 2011;44:1-23. https://doi.org/10.2190/EC.44.1.a Article
- 41. Wester ER, Walsh LL, Arango-Caro S, Callis-Duehl KL. Student engagement declines in STEM undergraduates during COVID-19-driven remote learning. J Microbiol Biol Educ 2021;22:22.1.50. https://doi.org/10.1128/jmbe.v22i1.2385 ArticlePubMedPMC
- 42. Chan SL, Lin CC, Chau PH, Takemura N, Fung J. Evaluating online learning engagement of nursing students. Nurse Educ Today 2021;104:104985. https://doi.org/10.1016/j.nedt.2021.104985 ArticlePubMed
- 43. Lee J, Song HD, Hong AJ. Exploring factors, and indicators for measuring students’ sustainable engagement in e-learning. Sustainability 2019;11:985. https://doi.org/10.3390/su11040985 Article
References
Figure & Data
References
Citations

- Online learning in Health Professions Education. Part 1: Teaching and learning in online environments: AMEE Guide No. 161
Heather MacNeill, Ken Masters, Kataryna Nemethy, Raquel Correia
Medical Teacher.2024; 46(1): 4. CrossRef - Research trends in e-learning practices for postgraduate medical education: A systematic review
Sinan Hopcan, Elif Polat, Ebru Albayrak
Education and Information Technologies.2024; 29(5): 5921. CrossRef - E‐learning and research experience exchange in the online setting of student peer mentor network during COVID‐19 pandemic and beyond: A laboratory case study
Dorota Lubanska, Sami Alrashed, Lia Oschanney, Alan Cieslukowski, Ali Nadi, Philip Habashy, Adam Renaud, Antonio Roye‐Azar, Mohamed Soliman, Kadila Adili, Allison Baker, Maliha Baseet, Amy Llancari, Aiden Mitrevski, Sahar Mouawad, Kim Nguyen, Alexandra So
Biochemistry and Molecular Biology Education.2024; 52(1): 93. CrossRef - Preparing Hematology/Oncology Fellows for Success: Implementing an Annual Career Development and Research Retreat
Akeem R. Lewis, Grace M. Choong, Elizabeth Cathcart-Rake, Narjust Florez, Urshila Durani, Siddhartha Yadav, Harry Fuentes, Karl Sorensen, Daniel S. Childs, Antoine Saliba, Jonas Paludo, Timothy J. Hobday
Journal of Cancer Education.2024; 39(1): 58. CrossRef - Development and Validation of an Active Educational Resource to Address Quality Gaps Regarding Clinical Documentation
Cailee E. Welch Bacon, Sara L. Nottingham, Tricia M. Kasamatsu
Athletic Training Education Journal.2024; 19(1): 1. CrossRef - Online teaching and learning of a pharmacy curriculum designed for active learning and professional skills development – A report of students' perceptions and learning experience in two international campuses
Suzanne Mary Caliph, Chooi Yeng Lee
Currents in Pharmacy Teaching and Learning.2024; 16(2): 119. CrossRef - Innovative practice in the training of future doctors
Ekaterina Bondarenko, Lyubov Khoronko, M.-T. Liong, I.V. Tkacheva
BIO Web of Conferences.2024; 84: 03030. CrossRef - Student satisfaction in clinical area subjects during the COVID-19 pandemic in a medical school
Anibal Diaz-Lazo, Aldo Alvarez-Risco, Carlo Córdova Rosales, Sandra Cori Rosales, Mely Ruiz-Aquino, Shyla Del-Aguila-Arcentales, Neal M. Davies, Christian R. Mejia, Jaime A. Yáñez
Frontiers in Education.2024;[Epub] CrossRef - Satisfaction and use of the didactic simulator for learning the nursing process: an observational study
Alberto Cruz-Barrientos, Eva Manuela Cotobal-Calvo, Ana María Sainz-Otero, José Manuel De-La-Fuente-Rodríguez, Daniel Román-Sánchez, Inés Carmona-Barrientos
BMC Nursing.2024;[Epub] CrossRef - Learning Environments in Undergraduate Nursing Education During COVID-19
Anna Lee, Sinhye Kim, Wonjung Noh
Nurse Educator.2024;[Epub] CrossRef - Novel teaching–learning and assessment tools to complement competency-based medical education in postgraduate training
Mohit K. Joshi
Indian Journal of Anaesthesia.2024; 68(1): 11. CrossRef - Assessment of parenteral dosage forms course objectives including objective structured practical examination by E-learning method
Faten Hamed, Tarek Jinani, Nisreen Mourad, Dalal Hammoudi Halat, Mohammad Rahal
Journal of Advanced Pharmacy Education and Research.2024; 14(1): 13. CrossRef - Dropout in online higher education: a systematic literature review
Amir Mohammad Rahmani, Wim Groot, Hamed Rahmani
International Journal of Educational Technology in Higher Education.2024;[Epub] CrossRef - Examining online international health professions education: a mixed methods review of barriers, facilitators, and early outcomes
Laura Dell’Aiera, David Fitzgerald, David Fisher, Norman W. Gill
The Journal of ExtraCorporeal Technology.2024; 56(1): 2. CrossRef - Swiss medical schools’ experiences with online teaching during the COVID-19 pandemic in light of international experiences
Artemisa Gogollari, Sharon Mitchell, Sissel Guttormsen
BMC Medical Education.2024;[Epub] CrossRef - Multi-disciplinary staff perspectives and consensus on e-Learning and mHealth for Health Sciences curricula
Habib Noorbhai, Danica Sims, Nadia Hartman
Higher Education Research & Development.2024; 43(3): 620. CrossRef - Evaluating Critical Thinking Disposition, Emotional Intelligence, and Learning Environment of Nursing Students: A Longitudinal Study
Antonios Christodoulakis, George Kritsotakis, Manolis Linardakis, Panayota Sourtzi, Ioanna Tsiligianni
Western Journal of Nursing Research.2024;[Epub] CrossRef - The Relationship between Academic Self-Efficacy and Motivation in the Online Nursing Education Process: The Mediator Role of Anxiety
Çiğdem Torun Kılıç, Bahar Candaş Altınbaş, Didem Sarımehmet, İlknur Buçan Kıkrbir
Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi.2024; 13(1): 119. CrossRef - The First Hybrid International Educational Comprehensive Cleft Care Workshop
Rami S. Kantar, Elçin Esenlik, Omar S. Al Abyad, Antonio Melhem, Robert A. Younan, Mario Haddad, Kristen Keith, Serena Kassam, Beyhan Annan, Charanya Vijayakumar, Arnaud Picard, Bonnie L. Padwa, Brian Sommerlad, Cassio Eduardo Raposo-Amaral, Christopher R
The Cleft Palate Craniofacial Journal.2023; 60(10): 1189. CrossRef - Bringing Psychology Students Closer to People with Schizophrenia at Pandemic Time: A Study of a Distance Anti-stigma Intervention With In-presence Opportunistic Control Group
Lorenza Magliano
Journal of Psychosocial Rehabilitation and Mental Health.2023; 10(3): 287. CrossRef - The effect of e-learning on point-of-care ultrasound education in novices
Wan-Ching Lien, Phone Lin, Chih-Heng Chang, Meng-Che Wu, Cheng-Yi Wu
Medical Education Online.2023;[Epub] CrossRef - Medical residents’ and teachers’ perceptions of the digital format of nation-wide didactic courses for psychiatry residents in Sweden: a survey-based observational study
Rajna Knez, Samir El Alaoui, Josefin Ivarson, Lise-Lotte Risö Bergerlind, Sarantos Stasinakis, Anna-Maria Ahlgren, Martin Maripuu, Danielle Talaee Mofrad, Klara Bolander Laksov, Nitya Jayaram-Lindström, Karolina Sörman
BMC Medical Education.2023;[Epub] CrossRef - Distance education as a tool to improve researchers’ knowledge on predatory journals in countries with limited resources: the Moroccan experience
Khalid El Bairi, Maryam Fourtassi, Rachid El Fatimy, Nadia El Kadmiri
International Journal for Educational Integrity.2023;[Epub] CrossRef - Developing as health professionals through community volunteering: exploring the value of a partnership between medical students and primary schools online compared to in-person
Alexandra M. Cardoso Pinto, Sajan B. Patel, Morwenna Stephens, Payal Guha, Ana Baptista, Susan Smith
BMC Medical Education.2023;[Epub] CrossRef - Radiography education in 2022 and beyond - Writing the history of the present: A narrative review
Y.X. Tay, J.P. McNulty
Radiography.2023; 29(2): 391. CrossRef - Self-determined motivation and associated factors among health professions students in distance learning: a cross-sectional study in Morocco
Aziz Naciri, Mohamed Radid, Hasnaa Sine, Ahmed Kharbach, Ghizlane Chemsi
Korean Journal of Medical Education.2023; 35(1): 33. CrossRef - Investigating medical students’ satisfaction towards video-based learning versus face-to-face lectures: a Jordanian tertiary teaching hospital experience
Omar Ashour, Ahmad Muneer Alkhatib, Qusai Al Zureikat, Mustafa Al-Shaikhli, Basel Bani Ata, Talal Massad, Leen Al-Huneidy, Mohammed Qussay Al-Sabbagh, Abdallah Al-Ani
Korean Journal of Medical Education.2023; 35(1): 21. CrossRef - Piloting a Telehealth Interprofessional Diabetes Clinic During Covid 19: Continuing patient care and student learning
Joan Pittman, Heather Brennan Congdon, Gina C. Rowe, Barbara Nathanson, Phyllis McShane, Rhonique Shields
Social Work in Health Care.2023; 62(2-4): 59. CrossRef - Standards for evaluating the quality of undergraduate nursing e-learning programme in low- and middle-income countries: a modified Delphi study
Moses Mutua Mulu, Champion N. Nyoni
BMC Nursing.2023;[Epub] CrossRef - Adaptación de la educación en enfermería a la modalidad en línea e híbrida durante la pandemia de COVID-19
Jéssica Patricia Salazar Menéndez, Esther Justina Ramírez García
LATAM Revista Latinoamericana de Ciencias Sociales y Humanidades.2023;[Epub] CrossRef - Evaluation of an Advanced Care Planning Training Program Incorporating Online Skills in Shared Decision Making: A Preintervention and Postintervention Comparative Study
Yuko Goto, Hisayuki Miura
Healthcare.2023; 11(9): 1356. CrossRef - The effect of COVID-19 pandemic on respiratory therapy students’ clinical practice: a cross-sectional study
Aseel Jamal Baoum, Elaf Asaad Hadidi, Renad Fahad Alharbi, Muhammad Anwar Khan, Alqassem Y. Hakami
BMC Medical Education.2023;[Epub] CrossRef - A SWOT Analysis of Pharmacy Students’ Perspectives on e-Learning Based on a Narrative Review
Carla Pires
Pharmacy.2023; 11(3): 89. CrossRef - ВИКОРИСТАННЯ ІНТЕРАКТИВНИХ ЗАСОБІВ НАВЧАННЯ ПРИ ВИКЛАДАННІ АНАТОМІЇ ЛЮДИНИ
Т. Я. Стравський, І. Є. Герасимюк, О. Я. Галицька-Хархаліс
Медична освіта.2023; (1): 82. CrossRef - Pharmacy Students’ Perceptions of Remote versus Face-to-Face Learning Experience
Jenna M. Mills, Celeste N. VanAtta, Racheal S. Hendershot, Shantanu Rao
Pharmacy.2023; 11(3): 97. CrossRef - Learning Outcomes and Educational Effectiveness of E-Learning as a Continuing Professional Development Intervention for Practicing Surgeons and Proceduralists: A Systematic Review
Erin Williams, Rosephine Del Fernandes, Ken Choi, Laurie Fasola, Boris Zevin
Journal of Surgical Education.2023; 80(8): 1139. CrossRef - Influence of Stress and Emotions in the Learning Process: The Example of COVID-19 on University Students: A Narrative Review
Alfredo Córdova, Alberto Caballero-García, Franchek Drobnic, Enrique Roche, David C. Noriega
Healthcare.2023; 11(12): 1787. CrossRef - The impact of Covid-19 on Moroccan students’ learning habits, mental health, and physical health (ENSA Fez as a case study)
Khawla Khoumssi, Asmae Achahbar
Social Science Information.2023; 62(2): 217. CrossRef - Understanding and Fostering Mental Health and Well-Being among University Faculty: A Narrative Review
Dalal Hammoudi Halat, Abderrezzaq Soltani, Roua Dalli, Lama Alsarraj, Ahmed Malki
Journal of Clinical Medicine.2023; 12(13): 4425. CrossRef - New innovations and educational process in undergraduate neurology education in blended learning
Siyu Mu, Jingman Hu, Fangxi Liu, Chuansheng Zhao, Yefei Sun
Postgraduate Medicine.2023; 135(6): 551. CrossRef - Knowledge, Use and Attitude of Information and Communication Technologies (ICTs) in Graduate Nursing Students: A Correlational Cross-Sectional Study
Alberto Cruz-Barrientos, Ines Carmona-Barrientos, Jose Manuel De-la-Fuente-Rodriguez, Veronica Perez-Cabezas, Gloria Gonzalez-Medina, Ana Maria Sainz-Otero
Healthcare.2023; 11(14): 1989. CrossRef - Understanding competency of nursing students in the course of case-based learning in Cambodia: a convergent mixed method study
Kyoko Koto-Shimada, Rogie Royce Carandang, Akira Shibanuma, Junko Kiriya, Ken Ing Cherng Ong, Sokneang Touch, Virya Koy, Masamine Jimba
BMC Nursing.2023;[Epub] CrossRef - Editorial: Public health promotion and medical education reform, volume II
Jing Tian, Jian Chen
Frontiers in Public Health.2023;[Epub] CrossRef - How are we doing with student-centered learning facilitated by educational technologies? A systematic review of literature reviews
Boulus Shehata, Ahmed Tlili, Ronghuai Huang, Michael Agyemang Adarkwah, Mengyu Liu, Tingwen Chang
Education and Information Technologies.2023;[Epub] CrossRef - South African health sciences students’ perspectives on utilisation, constraints and future possibilities of mHealth and e-Learning
Noorbhai Habib, Sims Danica, Hartman Nadia
Discover Education.2023;[Epub] CrossRef - Systematic review of distributed practice and retrieval practice in health professions education
Emma Trumble, Jason Lodge, Allison Mandrusiak, Roma Forbes
Advances in Health Sciences Education.2023;[Epub] CrossRef - Impact of COVID-19 on Dental Practices in El Salvador and Mexico: A Comprehensive Survey Analysis
Nuria Patiño-Marín, Wendy Yesenia Escobar de González, Katleen Argentina Aguirre de Rodríguez, Miguel Angel Casillas Santana, Carlo Eduardo Medina-Solís, Guillermo Alfonso Aguirre Escobar, Gabriel Alejandro Martínez-Castañón, Marco Salas
Cureus.2023;[Epub] CrossRef - Remote training for strengthening capacity in sexual and reproductive health and rights research: a systematic review
Carla Perrotta, Vicky Downey, Darin Elabbasy, Carolyn Ingram, Chungwan Lo, Amara Naseer, Anna Thorson, Vanessa Brizuela
BMC Public Health.2023;[Epub] CrossRef - Practical Strategies for Improving Sustainability and Scale-up of Noncommunicable Disease-related Public Health Interventions: Lessons from the Better Health Program in Southeast Asia
Tilahun Haregu, ShiangCheng Lim, Marcia Miranda, CongTuan Pham, Nam Nguyen, Inthira Suya, Rogelio Ilagan, Amphika Poowanasatien, Paul Kowal, Brian Oldenburg
WHO South-East Asia Journal of Public Health.2023; 12(1): 15. CrossRef - The Self-Perceived E-Learning Environment Scale: Development and Psychometric Properties in a Nursing Students Samples
Letizia Dal Santo, Marco Peña-Jimenez, Federica Canzan, Luisa Saiani, Adalgisa Battistelli
Nursing Education Perspectives.2023; 44(6): E39. CrossRef - The status of e-learning, personality traits, and coping styles among medical students during the COVID-19 pandemic: a cross-sectional study
Junfan Wei, Zhengcheng Yun, Yang Zhang, Xiaoxiao Mei, Li Ba, Huan Peng, Na Li, Meng Li, Zhu Liu, Hanjiao Liu
Frontiers in Psychiatry.2023;[Epub] CrossRef - The Learning Experience of Romanian Medical Students During the Online Teaching Imposed by the COVID-19 Pandemic
Dumitru Sutoi, Catalina Bazavan, Maria Sutoi, Alina Petrica, Adina Maria Marza, Cosmin Iosif Trebuian, Cosmin Librimir, Octavian Constantin Neagoe, Mihaela Ionica, Florina Buleu, Ovidiu Alexandru Mederle
Advances in Medical Education and Practice.2023; Volume 14: 1077. CrossRef - Change in the Learning Motivations and Attention Orientations of Students in the Pre- and Post-COVID-19 Periods: A Longitudinal Study
Mehmet PALANCI
International e-Journal of Educational Studies.2023; 7(15): 515. CrossRef - ПОЄДНАННЯ НОВІТНІХ ЦИФРОВИХ ТА КЛАСИЧНИХ МЕТОДІВ ПРИ ВИКЛАДАННІ АНАТОМІЇ ЛЮДИНИ у медичному закладі ВИЩОЇ ОСВІТИ
А. В. Мізь, І. Є. Герасимюк, Б. Я. Ремінецький
Медична освіта.2023; (2): 97. CrossRef - WPA Working Group on Medical Students: new accomplishments and online resources
Howard Y. Liu, Muhammad Waqar Azeem, Nazish Imran, Bernardo Ng, Khalid Bazaid, Pronob K. Dalal, Sridevi Sira Mahalingappa, Mohan Isaac, Afzal Javed
World Psychiatry.2023; 22(3): 491. CrossRef - e-Learning Evaluation Framework and Tools for Global Health and Public Health Education: Protocol for a Scoping Review
Awsan Bahattab, Michel Hanna, George Teo Voicescu, Ives Hubloue, Francesco Della Corte, Luca Ragazzoni
JMIR Research Protocols.2023; 12: e49955. CrossRef - Education and Training Adaptations for Health Workers during the COVID-19 Pandemic: A Scoping Review of Lessons Learned and Innovations
Perla Boutros, Nour Kassem, Jessica Nieder, Catalina Jaramillo, Jakob von Petersdorff, Fiona J. Walsh, Till Bärnighausen, Sandra Barteit
Healthcare.2023; 11(21): 2902. CrossRef - The Lancet Commission on medicine, Nazism, and the Holocaust: historical evidence, implications for today, teaching for tomorrow
Herwig Czech, Sabine Hildebrandt, Shmuel P Reis, Tessa Chelouche, Matthew Fox, Esteban González-López, Etienne Lepicard, Astrid Ley, Miriam Offer, Avi Ohry, Maike Rotzoll, Carola Sachse, Sari J Siegel, Michal Šimůnek, Amir Teicher, Kamila Uzarczyk, Anna v
The Lancet.2023; 402(10415): 1867. CrossRef - Can you teach a hands-on skill online? A scoping review of e-learning for point-of-care ultrasound in medical education
Maya Harel-Sterling
Canadian Medical Education Journal.2023;[Epub] CrossRef - An Online Learning Experience Simulating Video Telehealth with Older Adults: Student Perceptions
Megan E. Gately, Scott A. Trudeau
Journal of Technology in Behavioral Science.2023; 9(1): 154. CrossRef - Enhancement of Medical Students' Performance and Motivation in Pathophysiology Courses: Shifting From Traditional Instruction to Blended Learning
Dan Wang, Junhai Zhou, Qiuhui Wu, Guannan Sheng, Xin Li, Huiling Lu, Jing Tian
Frontiers in Public Health.2022;[Epub] CrossRef - Perceptions of Pharmacy Students on the E-Learning Strategies Adopted during the COVID-19 Pandemic: A Systematic Review
Carla Pires
Pharmacy.2022; 10(1): 31. CrossRef - ‘Learning in and out of lockdown’: A comparison of two groups of undergraduate occupational therapy students' engagement in online‐only and blended education approaches during the COVID‐19 pandemic
Ted Brown, Luke Robinson, Kate Gledhill, Mong‐Lin Yu, Stephen Isbel, Craig Greber, Dave Parsons, Jamie Etherington
Australian Occupational Therapy Journal.2022; 69(3): 301. CrossRef - Polysomnograph-e : un outil pédagogique en ligne pour l’apprentissage de la lecture des polysomnographies
M. Boulais, J.C. Comte, E. Stauffer, F. Gormand, I. Lambert, N. Limousin, R. Lopez, A. Leotard, A. Guyon, A. Raoux, M.J. Challamel, P. Franco, L. Peter-Derex
Médecine du Sommeil.2022; 19(3): 156. CrossRef - Study on the Academic Competency Assessment of Herbology Test using Rasch Model
Han Chae, Soo Jin Lee, Chang-ho Han, Young Il Cho, Hyungwoo Kim
Journal of Korean Medicine.2022; 43(2): 27. CrossRef - E-Learning in Clinical Chemistry: Indian Scenario
Prasenjit Mitra, Praveen Sharma
Indian Journal of Clinical Biochemistry.2022; 37(3): 255. CrossRef - Online-Offline Teaching for Bio-Pharmaceutical Students During the COVID-19 Pandemic: The Case Study of Advanced Mathematics in Application-Oriented Universities of China
Weicai Peng, Shuchao Wang
Frontiers in Public Health.2022;[Epub] CrossRef - The COVID-19 pandemic and its impact on medical teaching in obstetrics and gynecology—A nationwide expert survey among teaching coordinators at German university hospitals
Maximilian Riedel, Niklas Amann, Florian Recker, André Hennigs, Sabine Heublein, Bastian Meyer, Anne Karge, Gabriel Eisenkolb, Jacqueline Lammert, Anna Graf, Evelyn Klein, Martin Weiss, Fabian Riedel, Mohammed Saqr
PLOS ONE.2022; 17(8): e0269562. CrossRef - Educational impact of an active learning session with 6-lead mobile electrocardiography on medical students’ knowledge of cardiovascular physiology during the COVID-19 pandemic in the United States: a survey-based observational study
Alexandra Camille Greb, Emma Altieri, Irene Masini, Emily Helena Frisch, Milton Leon Greenberg
Journal of Educational Evaluation for Health Professions.2022; 19: 12. CrossRef - An evaluation of undergraduate student nurses' gameful experience whilst playing a digital escape room as part of a FIRST year module: A cross-sectional study
Isabel Antón-Solanas, Beatriz Rodríguez-Roca, Fernando Urcola-Pardo, Ana Anguas-Gracia, Pedro J. Satústegui-Dordá, Emmanuel Echániz-Serrano, Ana B. Subirón-Valera
Nurse Education Today.2022; 118: 105527. CrossRef - ProTransition – ein Online-Kurs für Fachkräfte zur Versorgungsoptimierung junger Menschen mit psychischen Störungen im Übergang zwischen Jugend- und Erwachsenenalter
Elisa König, Christina Stahl, Sandra Reetz, Ulrike M. E. Schulze, Jörg M. Fegert, Ulrike Hoffmann
Nervenheilkunde.2022; 41(09): 551. CrossRef - At the limits of digital education. The importance of practical education for clinical competencies learning in the field of emergency medicine: A controlled non-randomized interventional study
Lina Vogt, Michael Schauwinhold, Rolf Rossaint, Henning Schenkat, Martin Klasen, Saša Sopka
Frontiers in Medicine.2022;[Epub] CrossRef - Flexibel, zeit- und ortsunabhängig
Alexander Kraus, Patrick Mülleder, Verena Leinemann, Daniel Hausmann, Valentin Fischill-Neudeck, Peter Kaufmann, Patrizia Ebner, Jürgen Osterbrink
ProCare.2022; 27(6-7): 52. CrossRef - Students’ Experiences with Online Teaching and Learning in Norway: A Qualitative Study into Nutrition Education One Year after the COVID-19 Lockdown
Christine Tørris, Eli Gjølstad, Marianne Morseth, Jonas Debesay, Kari Almendingen
Education Sciences.2022; 12(10): 670. CrossRef - Factors influencing the E-learning system usage during the COVID-19 pandemic in Vietnam
Thang Xuân Do, Huong Thi Lan Tran, Thuy Thu Le, Ogochukwu Chinedum Okoye
PLOS ONE.2022; 17(12): e0278109. CrossRef - Factors affecting nursing and health technician students' satisfaction with distance learning during the COVID-19 pandemic in Morocco: a descriptive study
Aziz Naciri, Mohamed Radid, Abderrahmane Achbani, Mohamed Amine Baba, Ahmed Kharbach, Ghizlane Chemsi
Journal of Educational Evaluation for Health Professions.2022; 19: 28. CrossRef

 KHPLEI
KHPLEI


 PubReader
PubReader ePub Link
ePub Link Cite
Cite



