Articles
- Page Path
- HOME > J Educ Eval Health Prof > Volume 13; 2016 > Article
-
Research article
Does emotional intelligence influence success during medical school admissions and program matriculation?: a systematic review -
Christian Jaeger Cook1*†
 , Chad E. Cook2
, Chad E. Cook2 , Tiffany N. Hilton2
, Tiffany N. Hilton2
-
DOI: https://doi.org/10.3352/jeehp.2016.13.40
Published online: November 8, 2016
1Department of Biology, University of North Carolina, Chapel Hill, NC, USA
2Division of Physical Therapy, Department of Orthopedics, Duke University, Durham, NC, USA
- *Corresponding email: cjaegerc@live.unc.edu
Copyright © 2016, Korea Health Personnel Licensing Examination Institute
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Purpose
- It aimed at determining whether emotional intelligence is a predictor for success in a medical school program and whether the emotional intelligence construct correlated with other markers for admission into medical school.
-
Methods
- Three databases (PubMed, CINAHL, and ERIC) were searched up to and including July 2016, using relevant terms. Studies written in English were selected if they included emotional intelligence as a predictor for success in medical school, markers of success such as examination scores and grade point average and association with success defined through traditional medical school admission criteria and failures, and details about the sample. Data extraction included the study authors and year, population description, emotional intelligence I tool, outcome variables, and results. Associations between emotional intelligence scores and reported data were extracted and recorded.
-
Results
- Six manuscripts were included. Overall, study quality was high. Four of the manuscripts examined emotional intelligence as a predictor for success while in medical school. Three of these four studies supported a weak positive relationship between emotional intelligence scores and success during matriculation. Two of manuscripts examined the relationship of emotional intelligence to medical school admissions. There were no significant relevant correlations between emotional intelligence and medical school admission selection.
-
Conclusion
- Emotional intelligence was correlated with some, but not all, measures of success during medical school matriculation and none of the measures associated with medical school admissions. Variability in success measures across studies likely explains the variable findings.
- Processes involved with medical admissions commonly evaluate applicants based on cognitive and non-cognitive factors [1], with a majority associated with cognitive-intelligence factors. Because physicians often evaluate patient emotion and behavior when creating a treatment plan, having a high degree of emotional intelligence may assist future physicians in patient care. Emotional intelligence is defined as “the ability to perceive emotions, to access and generate emotions so as to assist thought, to understand emotions and emotional knowledge, and to reflectively regulate emotions so as to promote emotional and intellectual growth” [2]. To our knowledge, there are no systematic reviews that have explored the predictive capacity of emotional intelligence for success in being admitted and during matriculation of medical school. The purpose of this study was to determine whether emotional intelligence is a predictor for success in a medical school program and whether the emotional intelligence construct correlated with other markers for admission into medical school.
Introduction
- Study design
- This systematic review used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [3]. The PRISMA guidelines are commonly used for multiple forms of research methodologies [4]. The authors also worked with a biomedical librarian on all search processes.
- Eligibility criteria
- Inclusion criteria required the following items: first, a study that explicitly examined emotional intelligence as a predictor for success during matriculation in medical school; second, markers of success that were defined by written examination scores, continuous assessments, final examinations, weighted grade point average (wGPA), and association with success defined through traditional medical school admission criteria and failures; third, details provided about the sample including demographics, etc.; and fourth, published in English. Excluded papers were those that were examined a single construct of emotional intelligence (e.g., empathy).
- Information sources
- Three databases were used during the search strategy: PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Education Resources Information Center (ERIC). All three were searched from their establishment to July 2016.
- Search
- Search terms used in the systematic review were (MH “school admissions+”) AND (MH “emotional intelligence”) in CINAHL, “School admission criteria” [MeSH terms] OR “medical school” [all fields] AND “emotional intelligence” [MeSH terms] in PubMed, and Admission criteria and emotional intelligence in ERIC. Key terms used in each search included: school admissions, medical school, emotional intelligence, and admission criteria. The search was designed to be sensitive, and not specific, since emotional intelligence is recent terminology within the medical search engines.
- Study selection
- One author (CJC) performed a title screen and abstract review in PubMed. Two authors (CJC and CEC) then completed full-text reads to determine appropriateness for inclusion of each article, with a 100% consensus. The same screening process was repeated in CINAHL and ERIC, with duplicate articles removed when found. One author (CEC) also performed a hand search of references from the included papers.
- Data collection process
- One author (CJC) read each of the studies for associations between emotional intelligence scores and the measured success subjects experienced in medical school, along with associations between emotional intelligence and traditional selection measures. This author extracted the relevant data, noting the statistical relationships to emotional intelligence.
- Data items-emotional intelligence measures
- The study included any papers with explicit mechanisms to evaluate emotional intelligence in self-report format. We considered the measures of Mayer-Salovey-Caruso Emotional intelligence Test (MSCEIT) [5], Situational Test of Emotional Understanding (STEU) [6], Situational Test of Emotion Management (STEM) [6], and the Emotional Intelligence Inventory (EQ-I) [7] as qualifying emotional intelligence measures. The MSCEIT is an ability-based test created to measure the four branches of the emotional intelligence model that was developed by Mayer et al. [5] and consists of 141 items and takes 30–45 minutes to complete, providing 15 main scores: total emotional intelligence score, two area scores, four branch scores, and eight task scores [5]. The STEU is a test developed by MacCann and Roberts [6] that examines emotional understanding, a key component of emotional intelligence. The test-taker is required to choose which five emotions is most likely to result from an emotional situation in each item. STEM, a test also developed by MacCann and Roberts [6], assesses emotion management, the capacity of individuals to regulate their emotions by reducing negative feelings and enhancing positive ones. Subjects are given a situation then must choose from four strategies to apply to improve emotions and manage the problem. EQ-I [7] was developed to assess the Bar-On model of emotional-social intelligence. This test is a self-report measure designed to examine a number of constructs related to emotional intelligence, consisting of 133 items and taking approximately 30 minutes to complete.
- Data items-outcomes measures
- We accepted medical school success measures such as written examination scores, continuous program-based assessments, final examinations, wGPA, and failures such as failing grades and dropouts. With respect to medical school admission assessments, we accepted scores on interviews, Undergraduate Medicine and Health Sciences Admission (UMAT) scores, Tertiary Entrance Rank (TER), wGPA, and autobiographical test scores. UMAT is an admissions test that was developed by the Australian Council for Educational Research and used to assist with selection of students into the medicine, dentistry and health science degree programs at undergraduate level. The TER was a tertiary entrance score used as a tool for selection to universities in Australia that was replaced by the Australian Tertiary Admission Rank in 2010, in all territories except Queensland. The wGPA is a grade point average that takes into account the difficulty of classes and increases accordingly. Autobiographical scores could include materials such as personal statements, essays, and letters.
- Risk of bias in individual studies
- Methodological quality was assessed by one author (CJC) using the Newcastle-Ottawa Scale [8] for assessing the quality of nonrandomized studies in meta-analyses. A ‘star system’ is used through which a study is judged based on three broad perspectives: the selection of the study groups; the comparability of the groups; and the method of achieving the outcome of interest for cohort studies (Appendix 1).
- Risk of bias across studies
- Risk of bias across studies was evaluated by examining grey literature, conference proceeding, and other environments to identify research on emotional intelligence and medical admissions that had not been formally published.
- Strength of association parameters
- Strength of association measures included any acceptable correlation coefficient (measure used depended on the data used), which represents the strength of the presumed linear association between the variables in question, and ranges from −1 to +1 [9]. A correlation coefficient of zero indicates that no linear relationship exists between two tested variables, whereas a value closer to +1 suggests a positive correlation and a value of -1 suggests a negative correlation.
- Ethical approval
- This study was exempt from the local institutional human ethics review board of both institutions.
Methods
- Study selection
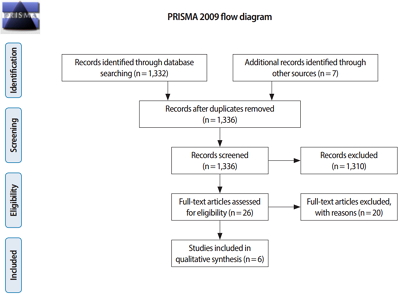
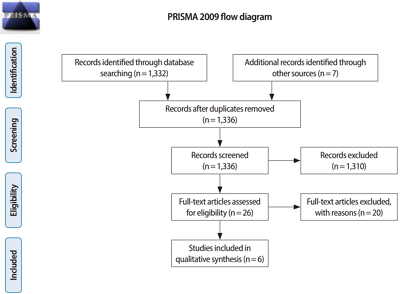
- In total, 1,332 articles were initially identified through database search of PubMed, CINAHL, and ERIC. A hand search also resulted in seven articles. Once duplicates were removed, a total of 1,336 articles remained. After title screening and abstract review, 26 articles were pulled and reviewed in full. The final search yielded six manuscripts [10,11,12,13,14,15], analyzing emotional intelligence as a predictor for success in medical school or as a predictor for medical school admissions [16] (Fig. 1).
- Study characteristics
- Total population across all studies was found to be 1,859 (range, 51 to 659). Three of the studies [10,11,12] were longitudinal and three were cross-sectional [13,14,15]. The medical students who participated in the studies included undergraduate medical students (i.e., Australia), graduate medical students, and those applying to and then matriculating into medical school. Success in medical school was defined in these studies by clinical competency assessments, bio-medical knowledge based assessments, scores on written examinations, objective structures clinical examinations (OSCEs), the number of nominations for excellence in clinical performance, number of failures, interpersonal academic performance, intellectual academic performance, tests of cognitive ability, continuous assessments, and final examinations (Table 1).
- There were four tools used to measure emotional intelligence. These tools included: the MSCEIT [11,12,13,14,15]; EQ-I [11]; the STEU and the STEM [10]. Emotional intelligence was compared as a predictor to success to the UMAT [13], interview, TER scores [13], and other traditional measures such as wGPA and autobiographical sketch scores.
- Risk of bias within studies
- The second question of the Newcastle-Ottawa Scale was excluded as it was not applicable to the design of the studies. Because of the way in which emotional intelligence is measured, the ascertainment of emotional intelligence scores among all studies were considered written self-reports. Most studies lacked controls, with the exception of one in which nonresponse bias was controlled for by having applicants respond as part of their medical school curriculum. Further trends included a lack of adequate follow-up in all but one study; however, minimal follow-up was still long enough for outcomes to occur. All but one study assessed the outcomes through record linkage. Outcomes of interest (success in medical school or a correlation between emotional intelligence and traditional measures of acceptance) appeared not to be present at the start of any studies. All studies were similar in their results of risk of bias assessment (Table 2).
- Synthesized results of studies-success while matriculated
- Four studies [10,11,12,14] examined emotional intelligence as a predictor for success in medical school. One study was cross-sectional [14], the remaining were longitudinal [10,11,12]. Chew et al. [14] found that students who were more emotionally intelligent tended to perform better in both the continuous assessments (r=0.24, P=0.003) and the final professional examination (r=0.21, P=0.01). Libbrecht et al. [10] found that emotional intelligence correlated positively with interpersonal academic performance (r=0.21, P<0.001). Humphrey-Murto et al. [12] found no significant correlations when evaluating associations between scores on the MSCEIT and written examination scores for interview and matriculated studies in two cohorts but did find a statistically significant positive correlation between the year 4-total OSCE score and the MSCEIT score (r=0.35, P<0.001). A final study [11] found that at first assessment EQ-I scores were negatively associated with performance on the clinical competency modules (r=-0.38, P<0.01). At a second assessment, an association between EQ-I scores and poor performance on the clinical competency module were found once again [11] (Table 1).
- Synthesized results of studies-medical school admission
- Two studies [13,15] examined traditional medical school admissions criteria and how it related to emotional intelligence; both studies were cross-sectional. One study found no significant correlations between emotional intelligence total and any of the selection scores for the first cohort [13]. The second study found a lack of substantial relationships between emotional intelligence scores and traditional medical school admission measures [15].
- Risk of bias across studies
- There were no instances in which grey literature was found, suggesting no publication bias. There were also no instances of selective reporting among accepted studies.
Results
- The aim of this study is to gather all data about emotional intelligence as a predictor for success in medical school or admissions into medical school. Key findings were as follows: first, three of the four studies [10,12,14] appear to support a weak positive relationship between emotional intelligence and academic performance upon matriculation into a program; second, one study [11] that reported a weak negative relationship between emotional intelligence scores and success during matriculation; and third, no relationship between emotional intelligence measures and admissions criteria used in medical school selection. We posit that there are a number of reasons that the evidence is mixed.
- As a whole, measures of success varied markedly across studies. While some studies based success on hard scores received from commonly used methods (written tests), others were more subjective or were based on professional development criteria. This subjectivity in the measures of success could be the cause for why no relationship was found between emotional intelligence and indicators for success in the respective studies. Other differences among studies included study populations make up and size, graduate status, locations, and assessment time (cross sectional and longitudinal).
- As stated, three of four papers [10,12,14] found statistically significant relationships between emotional intelligence and academic success while matriculated into the program. However, the strengths of the associations were small, often close to zero, suggesting a weak linear relationship. Further, most studies used multiple measures with only a few finding statistical significance. Nearly all studies used simple associational statistical analyses and finding statistical significance with large samples, despite weak relationships is a known conundrum [17]. Interestingly, some scores were significant only at given timeframes throughout the longitudinal testing dates despite using similar measures of success.
- When measures of success for admissions were evaluated we found no statistically significant associations [13,15]. Admissions measures included wGPA, which was calculated using the three most recent years of full-time undergraduate studies and autobiographical sketch scores. Interview scores were found when the applicants underwent independent interviews [15]. Emotional intelligence was also compared against the TER and the UMAT. The TER is the sum of the four highest courses of study scores obtained at the end of high school. Researchers suggest that TER is the strongest predictor for success in early medical school, though not as strong in predicting workplace success.
- One concern about measuring emotional intelligence is the limitations associated with the tool itself. Almost every study used the MSCEIT as a measure for emotional intelligence. While having a consistent way to measure emotional intelligence is beneficial, the test itself is based on the self-reporting of the participants, which in situations that subjects are aware that they are being evaluated, can lead to self-reporting biases. Because all emotional intelligence scores are derived by self-report of the participants in the study, their respective emotional intelligence scores may not entirely be accurate representations of the participant’s true emotional intelligence. Furthermore, because the study relies on its participants to respond on their own volition, nonresponse bias can occur. Only one study succeeded in a 100% response rate, due to the study being interwoven as part of a requirement for the curriculum of the medical students [10].
- After synthesizing the evidence as presented, we are skeptical that the current tools adequately capture the complex construct associated with emotional intelligence. Since the value of measuring this construct is to identify those who will be successful within an academic medical program or after graduation from a medical program, we would argue that the tools do not exclusively meet this assumption. In particular, we suggest the following inadequacies deserve attention: first, emotional intelligence is typically measured as a stand-alone construct and it likely interacts with multiple other measures of success; second, the current methods used to capture emotional intelligence may allow one to artificially elevate their scoring; thus reducing a potential effect of this construct; and third, the success criteria used was markedly different across studies, leading to notable variability in measurements across studies so that future research studies should include uniform accepted criteria to reduce variability.
- This study was limited to English only journals and we were limited in synthesizing the data since the success and predictor (emotional intelligence) variables were markedly different among studies. Furthermore, population differences suggest that compiling findings is unwarranted. Much more work is necessary before incorporating or dismissing the current tools. Future studies should use accepted criteria for success and explore interactions with other markers of success.
Discussion
-
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Article information
Acknowledgments
Supplementary materials
| Author | Population description | Emotional intelligence tool | Outcome variable | Results |
|---|---|---|---|---|
| Carr [13] (2009) | 177 Senior medical students from year 5 and 6 of a 6-year undergraduate curriculum. | MSCEIT | UMAT, interview, and TER scores | No significant correlations were found between EI total or EI branch scores and any of the selection scores (UMAT, TER, and interview) |
| Chew et al. [14] (2013) | 163 Medical students, 84 in the first-year and 79 in the final-year. | MSCEIT | Continuous assessments or final examinations | Students who were more emotionally intelligent performed better in both the continuous assessments and the final professional examination. |
| Doherty et al. [11] (2013) | 51 Graduate entry medical students | Emotional Intelligence Inventory and MSCEIT | Clinical competency assessments and bio-medical knowledge based assessments | High self-reported EI was found to be associated with poor performance on clinical competency assessments. |
| Humphrey-Murto et al. [12] (2014) | All applicants in 2006 and 2007 who were offered an interview at University of Ottawa (105 and 101 respectively) then again at matriculation (130 and 106, respectively). | MSCEIT | Scores on written examination and OSCEs. Also the number of nominations for excellence in clinical performance and failures recorded over the four years. | No significant correlations between MSCEIT scores and written examination scores or number of failures. Only MSCEIT scores at matriculation and OSCE year 4 scores for the 2007 cohort were significantly correlated. Correlations between MSCEIT scores and clinical nominations were low. Only the correlation between MSCEIT scores at matriculation and number of clinical nominations for the 2007 cohort were statistically significant. |
| Leddy et al. [15] (2011) | University of Ottawa medical school applicants of 2006 (333) and 2007 (326) who qualified for the admission interview. | MSCEIT | Traditional measures such as weighted grade point average, autobiographical sketch scores, and interview scores. | Lack of substantial relationships between EI scores and traditional medical school admission measures. |
| Librrecht et al. [10] (2014) | 367 Undergraduate medical students from a large European university who were followed up consecutively each year for 3 years. | Situational Test of Emotional Understanding and the Situational Test of Emotion Management | Interpersonal academic performance and intellectual academic performance along with tests of cognitive ability. | Positive correlation between EI and interpersonal academic performance. EI was not significantly related to intellectual academic performance. |
| Article | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Carr [13] (2009) | b | NA | c | a | None | b | a | d |
| Chew et al. [14] (2013) | a | NA | c | a | None | b | a | d |
| Doherty et al. [11] (2013) | b | NA | c | a | None | b | a | c |
| Humphrey-Murto et al. [12] (2014) | b | NA | c | a | None | b | a | d |
| Leddy et al. [15] (2011) | b | NA | c | a | None | c | a | d |
| Librrecht et al. [10] (2014) | b | NA | c | a | a | b | a | a |
1: Representativeness of the exposed cohort; 2: Selection of the non-exposed cohort; 3: Ascertainment of exposure; 4: Demonstration that outcome of interest was not present at start of study; 5: Comparability of cohorts on the basis of the design or analysis; 6: Assessment of outcome; 7: Was follow-up long enough for outcomes to occur; 8: Adequacy of follow up of cohorts.
NA, not applicable.
- 1. Ferguson E, James D, Madeley L. Factors associated with success in medical school: systematic review of the literature. BMJ 2002;324:952-957. https://doi.org/10.1136/bmj.324.7343.952 ArticlePubMedPMC
- 2. Mayer JD, Salovey P. What is emotional intelligence? In: Salovey P, Sluyter DJ, editors. Emotional development and emotional intelligence. New York (NY): Basic Books; 1997. p. 3-31.
- 3. Moher D, Liberati A, Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. https://doi.org/10.1136/bmj.b2535 ArticlePubMedPMC
- 4. Swartz MK. The PRISMA statement: a guideline for systematic reviews and meta-analyses. J Pediatr Health Care 2011;25:1-2. https://doi.org/10.1016/j.pedhc.2010.09.006 ArticlePubMed
- 5. Mayer JD, Salovey P, Caruso D. Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT): user’s manual. North Tonawanda (NY): Multi-Health Systems Inc.; 2002.
- 6. MacCann C, Roberts RD. New paradigms for assessing emotional intelligence: theory and data. Emotion 2008;8:540-551. https://doi.org/10.1037/a0012746 ArticlePubMed
- 7. Bar-On R. Bar-On emotional quotient inventory: technical manual. North Tonawanda (NY): Multi-Health Systems Inc.; 1997.
- 8. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses [Internet] Montreal: Faculty of Medicine; [cited 2016 Oct 2]. Available from: http://www.medicine.mcgill.ca/rtamblyn/Readings/The%20Newcastle%20-%20Scale%20for%20assessing%20the%20quality%20of%20nonrandomised%20studies%20in%20meta-analyses.pdf
- 9. Swinscow TD, Campbell MJ. Statistics at square one. 9th ed. London: BMJ Publishing Group; 1997.
- 10. Libbrecht N, Lievens F, Carette B, Cote S. Emotional intelligence predicts success in medical school. Emotion 2014;14:64-73. https://doi.org/10.1037/a0034392 ArticlePubMed
- 11. Doherty EM, Cronin PA, Offiah G. Emotional intelligence assessment in a graduate entry medical school curriculum. BMC Med Educ 2013;13:38. https://doi.org/10.1186/1472-6920-13-38 ArticlePubMedPMCPDF
- 12. Humphrey-Murto S, Leddy JJ, Wood TJ, Puddester D, Moineau G. Does emotional intelligence at medical school admission predict future academic performance? Acad Med 2014;89:638-643. https://doi.org/10.1097/ACM.0000000000000165 ArticlePubMedPMC
- 13. Carr SE. Emotional intelligence in medical students: does it correlate with selection measures? Med Educ 2009;43:1069-1077. https://doi.org/10.1111/j.1365-2923.2009.03496.x ArticlePubMed
- 14. Chew BH, Zain AM, Hassan F. Emotional intelligence and academic performance in first and final year medical students: a cross-sectional study. BMC Med Educ 2013;13:44. https://doi.org/10.1186/1472-6920-13-44 ArticlePubMedPMCPDF
- 15. Leddy JJ, Moineau G, Puddester D, Wood TJ, Humphrey-Murto S. Does an emotional intelligence test correlate with traditional measures used to determine medical school admission? Acad Med 2011;86(10 Suppl):S39-S41. https://doi.org/10.1097/ACM.0b013e31822a6df6 ArticlePubMed
- 16. Moher D, Liberati A, Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. https://doi.org/10.1371/journal.pmed.1000097 Article
- 17. Lin M, Lucas HC, Shmueli G. Too big to fail: large samples and the p-value problem. Inf Syst Res 2013;24:906-917. https://doi.org/10.1287/isre.2013.0480 Article
References
Appendix
Appendix 1.
Figure & Data
References
Citations

- Emotional intelligence weakly predicts academic success in medical programs: a multilevel meta-analysis and systematic review
Ahmed M. Abdulla Alabbasi, Fatema A. Alabbasi, Aseel AlSaleh, Ahmed M. Alansari, Reginald P. Sequeira
BMC Medical Education.2023;[Epub] CrossRef - Emotional intelligence in undergraduate medical students: a scoping review
Helga V. Toriello, J. M. Monica Van de Ridder, Patricia Brewer, Brian Mavis, Renoulte Allen, Cindy Arvidson, Iris Kovar-Gough, Elizabeth Novak, John O’Donnell, Janet Osuch, Brian Ulrich
Advances in Health Sciences Education.2022; 27(1): 167. CrossRef - Emotional Intelligence and Good Medical Practice: Is There a Relationship?
Cameron Dott, George Mamarelis, Edward Karam, Kavyansh Bhan, Kash Akhtar
Cureus.2022;[Epub] CrossRef - Concept Analysis of Emotional Intelligence in Nursing
Sun Yeob Choi
Journal of Korean Academy of Fundamentals of Nursing.2021; 28(2): 263. CrossRef - Medical Student Selection
Ian Kratzke, Muneera R. Kapadia, Fumiko Egawa, Jennifer S. Beaty
Surgical Clinics of North America.2021; 101(4): 635. CrossRef - Traits and Attributes of a Successful Physical Therapy Resident: A Delphi Study
Rebecca Shepard, Lauren Haines, Karen Abraham, A. J. Lievre
Journal of Physical Therapy Education.2021; 35(4): 315. CrossRef - Cross-Sectional Assessment of the Emotional Intelligence of Fourth-Year Veterinary Students and Veterinary House Officers in a Teaching Hospital
Darcy B. Adin, Kenneth D. Royal, Christopher A. Adin
Journal of Veterinary Medical Education.2020; 47(2): 193. CrossRef - Predictors of success on the MCAT among post-baccalaureate pre-medicine students
Rohini Ganjoo, Lisa Schwartz, Mackenzie Boss, Matthew McHarg, Yuliya Dobrydneva
Heliyon.2020; 6(4): e03778. CrossRef - More Than Their Test Scores: Redefining Success with Multiple Mini-Interviews
Ann Blair Kennedy, Cindy Nessim Youssef Riyad, Laura H. Gunn, April Gant Brown, Kandyce Brooke Dunlap, Melissa Elizabeth Knutsen, Alicia Anne Dahl
Medical Science Educator.2020; 30(3): 1049. CrossRef - COVID-19: A Driver for Disruptive Innovation of the Emergency Medicine Residency Application Process
Alexis Pelletier-Bui, Doug Franzen, Liza Smith, Laura Hopson, Lucienne Lutfy-Clayton, Kendra Parekh, Mark Olaf, Tom Morrissey, David Gordon, Erin McDonough, Benjamin Schnapp, Mary Ann Edens, Michael Kiemeney
Western Journal of Emergency Medicine.2020;[Epub] CrossRef - Reimagining Residency Selection: Part 3—A Practical Guide to Ranking Applicants in the Post-COVID-19 Era
Jaime Jordan, Kevan Sternberg, Mary R.C. Haas, Shuhan He, Lalena M. Yarris, Teresa M. Chan, Nicole M. Deiorio
Journal of Graduate Medical Education.2020; 12(6): 666. CrossRef - Assessments of Non-academic Attributes in Applicants for Undergraduate Medical Education: an Overview of Advantages and Limitations
Jochanan Benbassat
Medical Science Educator.2019; 29(4): 1129. CrossRef - The right kind of smart: emotional intelligence’s relationship to cognitive status in community-dwelling older adults
Odelyah Saad, Leehu Zysberg, Jeremia Heinik, Ron Ben-Itzhak, Anna Zisberg
International Psychogeriatrics.2019; 31(9): 1241. CrossRef - The relationship between emotional intelligence, previous caring experience and successful completion of a pre‐registration nursing/midwifery degree
Austyn Snowden, Rosie Stenhouse, Lorraine Duers, Sarah Marshall, Fiona Carver, Norrie Brown, Jenny Young
Journal of Advanced Nursing.2018; 74(2): 433. CrossRef - A novel tool for evaluating non-cognitive traits of doctor of physical therapy learners in the United States
Marcus Roll, Lara Canham, Paul Salamh, Kyle Covington, Corey Simon, Chad Cook
Journal of Educational Evaluation for Health Professions.2018; 15: 19. CrossRef - 20th Pauline Cerasoli Lecture: The Sunk Cost Fallacy
Chad Cook
Journal of Physical Therapy Education.2017; 31(3): 10. CrossRef - What is interesting in the issue 2016 of Journal of Educational Evaluation for Health Professions?
Yera Hur
Journal of Educational Evaluation for Health Professions.2016; 13: 46. CrossRef

 KHPLEI
KHPLEI

 PubReader
PubReader ePub Link
ePub Link Cite
Cite